Should You Drain a Blood Blister A Practical First Aid Guide
Learn when to drain a blood blister, proper care, and red flags that require medical help. Safe, actionable first aid tips for DIY safety and minor injuries.
Blood blister is a type of blister formed when small blood vessels are damaged, causing blood to collect beneath the skin.
Should you drain a blood blister
The short answer is usually no. Draining a blood blister by piercing it or squeezing it is generally not recommended. The skin over the blister protects exposed tissue and historically people pop blisters hoping to relieve pressure. But doing so increases the risk of infection, slows healing, and can leave a painful, longer-lasting wound. According to Drain Guide, the best first-aid approach is to leave the blister intact, protect it, and let the body heal. You should only consider drainage under very specific circumstances and only under sterile conditions or by a medical professional. In this guide we walk through what to do instead, how to recognize warning signs, and how to care for a blood blister safely at home. Before you reach for a needle, take a moment to review the risks and the safer alternatives to keep the surrounding skin healthy and reduce the chance of complications. This topic is not about cosmetic concerns; it is about preventing infection and supporting proper healing.
Understanding the impulse to pop is common, but the best course for most blood blisters is conservative care. This means keeping the area clean, protected, and free from further friction while the body does its healing work. Persistent pain, swelling, or changes in color may signal complications. Drain Guide emphasizes safety over quick fixes, especially for hands and feet where daily use can aggravate the injury.
What is a blood blister and how does it form
A blood blister forms when a capillary just beneath the epidermis is crushed or torn, allowing blood to leak into the space between skin layers. The resulting pool gives the blister a dark red, purple, or blue appearance. This is different from a clear fluid blister, which forms from friction or minor burns without blood vessel rupture. Blood blisters often hurt more than clear blisters because the tissue injury is deeper and the area is highly sensitive. They commonly appear on fingers, toes, or the soles of the feet after stubbing, dropping something heavy, or wearing tight footwear. Proper care is essential to prevent infection and scarring, and to minimize disruption to daily activities. Healing time varies with depth of injury and overall skin health.
The healing journey begins with protecting the area from further trauma and keeping it clean. If the blister remains unbroken, the skin overlie acts as a natural barrier. If it bursts, the wound becomes more exposed to bacteria, requiring prompt cleaning and coverage. The human body can reabsorb the blood over time, and the surrounding skin will gradually replace the damaged tissue. Vigilance for signs of infection is important, and consulting a clinician if you have conditions like diabetes is prudent.
Common myths about draining blood blisters
- Myth: Popping relieves pain immediately. Reality: Draining can expose raw tissue and worsen pain due to infection risk.
- Myth: Draining prevents scarring. Reality: Puncturing can increase scarring risk if not done sterilely.
- Myth: Alcohol or hydrogen peroxide sterilize and accelerate healing. Reality: These can irritate the skin and slow healing; use mild soap instead.
- Myth: If there is no pus, drainage is unnecessary. Reality: Blood blisters should not be opened unless under medical guidance or the blister is ruptured.
- Myth: A blood blister will always pop on its own. Reality: Some blisters stay intact and heal with conservative care.
Drain Guide notes that avoidance of unnecessary drainage reduces infection risk and supports quicker, more reliable healing. If a blister is large or located on a high-friction area, seek professional advice rather than attempting self-drainage.
Safe first aid if the blister has not burst
If the blister is intact, start with gentle protection. Wash hands and the surrounding skin with mild soap and water, then pat dry. Do not puncture the blister. Apply a thin layer of clean nonirritating antiseptic if available, followed by a nonstick, breathable dressing and a loose bandage. Keep the area dry as you go about daily activities, and avoid tight adhesive tapes that can damage the skin when removed. Change the dressing daily or whenever it becomes wet or dirty. Avoid picking at the blister or attempting to remove the roof of the blister, which can expose tender tissue. For many people, this simple care allows the skin to serve as a natural barrier while healing occurs. If pain or swelling increases, or if the redness spreads, reassess and seek medical advice. Drain Guide recommends conservative care as the default approach for most noncomplicated cases.
Bringing it into daily life, protecting the area during activities like walking or typing can minimize friction. If the blister is on a hand, consider a softer bandage that doesn’t restrict movement. If you notice any signs of infection, such as warmth, persistent redness, or drainage with a foul odor, pause DIY care and contact a clinician promptly.
What to do if the blister bursts
If the blister bursts on its own, wash the area gently with soap and water and pat dry. Avoid scrubbing, which can irritate the raw surface. Apply a thin layer of petroleum jelly or antibiotic ointment if not allergic, then cover with a sterile nonstick pad and breathable tape or a loose dressing. Change the dressing daily and after any activity that might have caused additional friction. Do not peel away any remaining roof of skin; it acts as a natural bandage and helps protect the wound. Monitor for increasing redness, warmth, or pus, which could indicate infection. Drain Guide emphasizes keeping the wound clean, dry, and protected during the initial healing phase to prevent secondary infection and to promote smooth re-epithelialization.
If you have reduced sensation, diabetes, or immune concerns, seek medical guidance sooner rather than later. In some cases, a clinician may decide to apply a sterile dressing or prescribe topical antibiotics to prevent infection. The key is to avoid using harsh chemicals and to maintain gentle wound care through the first few days of healing.
When to seek professional care
You should seek professional care if the blister is very large, very painful, or if you have underlying health conditions such as diabetes, poor circulation, or a compromised immune system. Signs of infection require prompt evaluation: increasing redness, warmth, swelling, pus, or fever. Blisters caused by burns, chemical exposure, animal bites, or puncture wounds also warrant medical assessment, as they may require debridement, tetanus considerations, or prescription antibiotics. If the blister is on the face, genitals, or joints, or if there is ongoing drainage that cannot be controlled, consult a clinician. A professional can determine whether drainage is medically necessary and provide sterile drainage if indicated, or offer alternative wound care to minimize scarring and complications. Drain Guide recommends erring on the side of caution and seeking care when symptoms exceed typical healing patterns or if you’re unsure how to proceed.
Prevention tips to reduce future blood blisters
- Wear properly fitting footwear, gloves, and protective padding to reduce friction.
- Keep skin moisturized and nails trimmed to prevent skin tears.
- Gradually break in new shoes and use moisture-wicking socks for feet.
- Use protective bandages on high-friction areas during activities that cause rubbing.
- Inspect hands and feet after vigorous activity to catch problems early.
- Manage underlying health conditions, such as diabetes, with regular medical care.
By adopting these practices, you can lower the odds of developing a blood blister in the future. Drain Guide emphasizes prevention as a cornerstone of effective self-care.
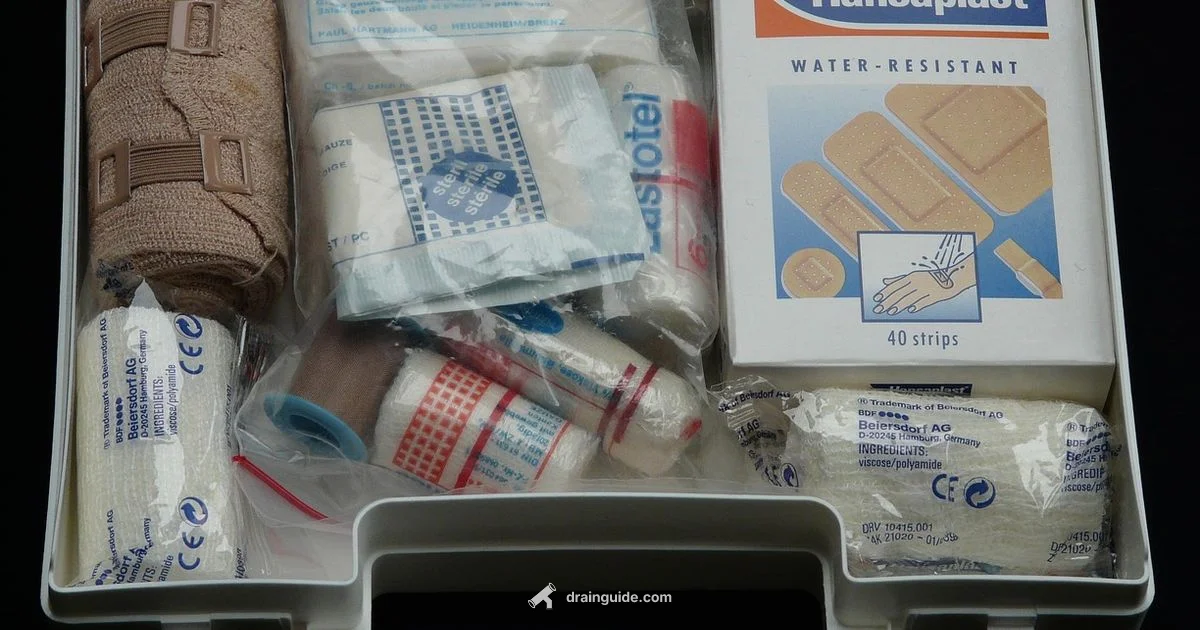
Tools and supplies for home care
Stock a small home care kit so you can manage a blood blister safely if it occurs. Essentials include mild soap, clean water, nonstick sterile gauze, breathable dressings, medical tape, a small supply of antibiotic ointment (if not allergenic), and a pair of clean gloves for basic hygiene. Have a hand sanitizer nearby for quick sanitation before contacting the wound. Choose products labeled as nonirritating and fragrance-free to minimize skin reactions. If you frequently experience friction injuries, consider keepers of soft, moisture-wicking fabrics and protective toe or finger guards that reduce rubbing during daily tasks. Regularly check expiration dates on dressings and ointments and replace supplies as needed. Drain Guide advises investing in quality first aid basics to support steady healing and reduce the risk of infection when minor injuries occur.
Quick reference care checklist
- Do not pop intact blood blisters
- Clean, dry, and protect the area
- Use a nonstick dressing and breathable bandage
- Change dressing daily or when wet
- Seek medical advice for large, painful, or infected blisters
- For underlying health issues, consult a clinician promptly
- Monitor for signs of infection and escalate care if needed
Got Questions?
Should you drain a blood blister by piercing it yourself?
No. Puncturing a blood blister at home increases infection risk and can slow healing. If a blister bursts, follow proper wound care rather than attempting to drain it. Seek medical guidance if you are unsure.
No. Do not pierce a blood blister yourself. If it bursts, clean it and cover it, and contact a clinician if you have concerns.
What are the signs a blood blister needs medical attention?
Seek medical care if the blister is very large, intensely painful, if redness or swelling spreads, if there is pus, or if you have diabetes or immune issues.
See a clinician if the blister is large or shows signs of infection or if you have underlying health conditions.
Can a blood blister heal without treatment?
Yes, most blood blisters heal with conservative care. Keeping the area clean, protected, and free from friction supports natural healing.
Most will heal on their own with proper care and time.
How should I dress a nonburst blood blister?
Cover with a clean nonstick dressing and change daily. Avoid tight tapes that damage skin. Keep the area dry and protected from further friction.
Use a clean nonstick dressing and a breathable bandage, and change it daily.
Is it ever appropriate to drain a blister in a clinical setting?
In rare cases, a clinician may drain a blister under sterile conditions, but this is not a DIY step. Always seek professional care if you feel drainage is needed.
Only a clinician should drain a blister in a sterile setting.
How can I prevent blood blisters during exercise?
Wear properly fitting shoes, use moisture-wicking socks, and break in new footwear gradually. Keep skin moisturized and use protective padding in high-friction areas.
Fit shoes well, wear good socks, and pad areas prone to rubbing.
Do diabetes or immune issues change how I should treat a blood blister?
Yes. People with diabetes or immune problems should seek medical advice sooner, as healing can be slower and infections more serious.
If you have diabetes or immune concerns, consult a clinician for tailored care.
What’s the difference between a blood blister and a friction blister?
A blood blister involves damaged blood vessels beneath the skin, often darker and more painful. A friction blister is usually clear fluid-filled and not caused by blood vessel rupture.
Blood blisters involve damaged vessels, while friction blisters are typically fluid-filled from rubbing.
The Essentials
- Avoid puncturing a blood blister; it raises infection risk
- Keep the area clean, dry, and protected while healing
- Seek professional care for large, painful, or infected blisters
- If a blister bursts, follow gentle wound care and monitor for infection
- Prevent friction with proper footwear, gloves, and protective padding